Contact Information
Research Areas
Metastasis, Precision medicine, Immunology & immunotherapy
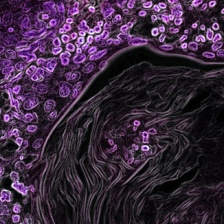
Our goal is to identify novel cancer drug targets, as well as strategies for tailoring drug regimens to target protective mechanisms used by cancers to evade and escape cancer therapy.
Research Summary
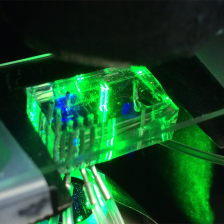
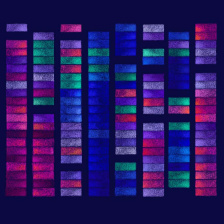
Many cancers have innate resistance to certain drugs, meaning that patients may be prescribed treatment regimens that are poorly suited to their particular case. Other times, cancers that initially respond favorably to a given treatment eventually acquire resistance, leading to relapse. The Hemann Laboratory approaches this key challenge in cancer treatment from a number of angles, with the goal of improving personalized medicine and patient outcomes. The lab uses high-throughput screening technology, in combination with tractable pre-clinical mouse models, to investigate basic mechanisms of intrinsic and acquired drug resistance. Through the use of genetic and computational tools, the Hemann group also works to understand how cancer therapies exert their effects, and how to best combine drugs in order to improve efficacy and preempt evolution of chemoresistance. Their overall goals are to identify novel cancer drug targets and strategies for tailoring drug regiments to overcome the protective mechanisms used by cancers to evade and escape cancer therapy.
Biography
Michael Hemann is an associate professor in MIT’s Department of Biology, a member of the Koch Institute, and an associate member of the Broad Institute. He earned his bachelor’s degree in molecular biology and biochemistry from Wesleyan University in 1993, and a doctorate in human genetics from the Johns Hopkins University School of Medicine in 2001. For his doctoral work, he was awarded the Harold M. Weintraub Graduate Student Award from the Fred Hutchinson Cancer Research Center. He was a post-doctoral fellow in the laboratory of Scott Lowe at Cold Spring Harbor Laboratory in New York, where he was supported by a Helen Hay Whitney Fellowship and a Lauri Strauss Leukemia Foundation Grant. Since his arrival at MIT in 2006, he has been awarded a V Foundation Fellowship and was selected as a Rita Allen Scholar.